Finger Deformity
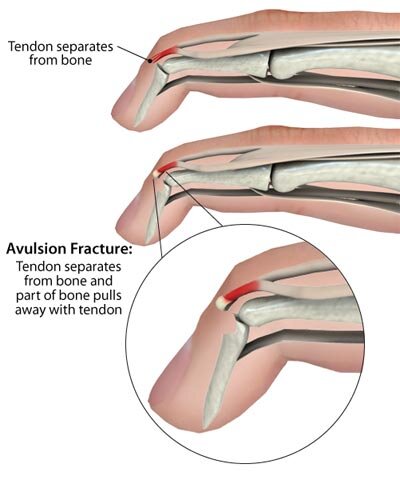
Mallet Finger
Finger deformity caused by disruption of the terminal extensor tendon distal to DIP joint
may be bony or tendinous: Xrays are needed
Treatment
extension splinting of DIP joint for 6-8 weeks for 24 hours daily
for soft tissue injury or for non displaced bony avulsion
avoid hyper-extension
PIP joint must be FREE
Surgery
ORIF or percutaneous
Indications
volar subluxation of distal phalanx
>50% of articular surface involved ( relative indication)
>2mm articular gap ( relative indication)
Surgical reconstruction for chronic cases ( if normal joint, but results not so good)
DIP arthrodesis ( if painful joint)
Finger splint
Wire
Tenodermodesis
Swan Neck Deformity
Characterized by
hyperextension of PIP
flexion of DIP
Caused by
Primary lesion: lax volar plate
Secondary lesion: imbalance of muscle forces on PIP (extension force > flexion force)
MCP joint volar subluxation (rheumatoid arthritis)
Mallet finger
FDS laceration
Intrinsic contracture (Seen in rheumatoid arthritis)
Treatment
Conservative : double ring splint (to prevent hyper extension of PIP)
Surgical: volar plate advancement and correct PIP joint muscles imbalances with either
Central slip tenotomy (Fowler) : most used
FDS tenodesis indicated with FDS rupture
Spiral oblique retinacular ligament reconstruction
Xray showing the deformity: PIP hyperextension and PID flexion
Double ring splint
Double ring splint
Boutonniere Deformity
Deformity characterized by
PIP flexion
DIP extension
Caused by rupture of the central slip over PIP joint from (laceration, traumatic avulsion (jammed finger),
capsular distension in rheumatoid arthritis
pathoanatomic sequence includes
rupture of central slip
attenuation of triangular ligament and palmar migration of collateral bands and lateral bands
causes intrinsic muscles of the hand (lumbricals) to act as flexors at the PIP joint
lumbricals also extend the DIP joint without an opposing or balancing force
Associated conditions
rheumatoid arthritis
pseudo-boutonniere: refers to PIP joint flexion contracture in the absence of DIP extension
Physical exam
Deformity
Elson test is the most reliable way to diagnose a central slip injury before the deformity is evident
Treatment
Nonoperative
splint PIP joint in full extension for 6 weeks
indications
acute closed injuries (< 4 weeks)
technique
encourage active DIP extension and flexion in splint to avoid contraction of oblique retinacular ligament
complete part-time splinting for an additional 4-6 weeks
Operative
primary central band repair
indications
acute displaced avulsion fx (proximal MP avulsion seen on x-ray)
open wound that needs exploration
lateral band relocation vs. terminal tendon tenotomy vs. tendon reconstruction
indications
in chronic injuries after FROM is obtained with therapy or surgical release
technique
terminal tendon tenotomy (modified Fowler or Dolphin tenotomy)(never central slip tenotomy)
secondary tendon reconstruction (tendon graft, Littler, Matev)
triangular ligament reconstruction
PIP arthrodesis
indications
rheumatoid patients
painful, stiff and arthritic PIP joint